Programmable off-the-shelf dendritic cells as an immunotherapy discovery platform
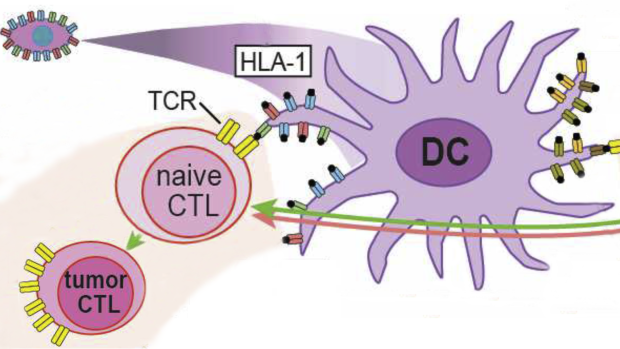
Dendritic cells (DC) regulate diverse processes in the human immune system. An off-the-shelf DC, programmed with so-called human leukocyte antigens (HLAs) and tumor-specific antigens would have broad uses in many areas of immunotherapy, including cancer. The figure shows how DCs provide pro- and anti-immune functions involving cytotoxic T lymphocytes (CTLs) with T-cell receptors (TCRs).
A new therapeutic era has been ushered in with Adoptive Cell Immunotherapy, which uses patient-harvested T cells genetically engineered against tumor-specific targets. However, the number of addressable cancers is limited by a lack of tumor-specific targets and T cell receptors.
A team led by David M. Truong, Ph.D., assistant professor of biomedical engineering, has been awarded a $1.8 million grant from the National Institute of Allergy and Infectious Diseases (NIAID) under the NIH Director’s New Innovator program, to address this issue by expanding the number of human leukocyte antigen (HLA) restricted T cell receptors (TCRs) and tumor-specific antigens (TSAs), thus transforming the entire immunotherapy pipeline.
To accomplish this, Truong proposes the generation of programmable Dendritic cells (DCs), which are professional antigen presenting cells that function to mature and activate naive T cells. These programmable DCs would facilitate the discovery of new TCRs, the validation of TSAs, and could even be used as “living” vaccines to marshal a patient’s own immune system against infectious disease and cancer.
Truong specifically hopes to produce off-the-shelf DCs pre-engineered to match any HLA haplotype, even rarer haplotypes, that are pre-encoded with any combination of TSAs. Truong’s group will search for and validate “universal” TSAs and TCRs that can be used broadly in TCR therapy for any patient.
More specifically, the group will focus on peptides expressed from regions of the genome which are normally epigenetically silenced, but which are reactivated in tumor cells, e.g., endogenous retroviruses. To further this, the group will continue to develop technology enabling the “writing” of millions of DNA base-pairs in human-induced pluripotent stem cells (iPSCs). Such technology allows for direct customization of the large HLA locus iPSCs in a single step, the introduction of libraries of potential TSAs, as well as integration of synthetic reporter constructs for safer and scalable directed differentiation of iPSCs to DCs.
This research on allogeneic programmed DCs may catalyze a wide variety of immunotherapy applications and expand access to advanced treatments for a greater number of patients.